A year on from the Aged Care Royal Commission’s damning final report, the Morrison Government has failed to take action to fix the embattled sector, says aged care assistant in nursing (AIN) Susan Walton.
A NSWNMA member, Susan has worked in the same residential aged care facility for the past 18 years. In 2019, she bravely gave evidence to the Aged Care Royal Commission, sharing her experience of working in the face of chronic understaffing.
An aged care advocate for almost two decades, when Susan began working in aged care she says the facility had “plenty of staff”. It was also well equipped with amenities including an in-house kitchen and organised numerous social activities for residents. Working under these conditions, she was able to spend quality time with residents and meet all of their care needs.
Over the years, however, standards declined, especially the number of trained staff.
“It’s just progressively got worse to where we now don’t have cooks or a kitchen, we don’t have cleaners, we don’t even have a laundry,” she explains.
“Most of our care staff’s gone. We’re on a skeletal crew and we’ve been like that for a long time. Then when COVID hit, we lost a small percentage [of staff] – our workforce has been decimated. It’s just not fair on the workers and especially our elderly residents.”
Susan typically looks after 40 residents on night shifts. She reveals there is lucky to be an RN on site to look after the facility’s 120 residents, with carers routinely forced to work outside of their scope and administer medication.
On her regular night shift, Susan heads in early to carry out a RAT test, which she pays for out of her own pocket. Masks and face shields are now part of the new normal.
Residents, ranging in complexity, are all housed together. Some experience dementia and problematic behaviours. Others are bed bound and need constant assistance.
“It’s just never-ending, you might have five or six buzzers going at a time and you have to decide who you think you can go to first,” says Susan.
“It’s declined so much now that if someone falls on the floor when I’m on night shift I wouldn’t know unless they’ve got an alarm mat because you do not have time physically to put eyes on 40 different people during the night. You’re too busy and then you’re drowning in paperwork.”
How did things get so bad?
Susan traces the aged care sector’s problems back to the 1997 Aged Care Act, implemented by the Howard Government, which overhauled the system and introduced partial privatisation.
“For starters, there’s no accountability for the billions of dollars that get provided [to providers]. Before John Howard changed it, every facility had to account for every single dollar they spent and that went on care and staff. It doesn’t go there now. They don’t even have to have a registered nurse on site.”
The COVID-19 pandemic has also exacerbated chronic understaffing in aged care, suggests Susan.
She says staff at her facility did not receive adequate training when the pandemic hit Australia.
“We didn’t have PPE, we didn’t have proper face masks, we didn’t have access to anything.”
As for residents, Susan says being confined to their rooms and unable to see loved ones for months on end has created social isolation and loneliness.
“It’s impacted them severely because most of them are really frightened and depressed. A lot of them don’t understand because they’re not seeing their loved ones every day.”
When Omicron infiltrated one of the organisation’s nearby facilities, Susan claims she was not informed by management, only finding out through a colleague.
“I went to work, I go in the basement and there’s a face shield there and a mask and the only communication I had was to write my name on the face shield, nothing about Omicron in the facility, nothing about the people I work with having Omicron and nothing about any of the residents,” she says.
“It’s very frightening. We’re all mentally, physically and emotionally exhausted and shattered.”
Susan says staff have only been given N95 masks to wear in recent weeks. But it’s a one-size-all approach with nobody fit-tested.
To support colleagues through the pandemic Susan, an active NSWNMA member, informs staff about their legal rights and upcoming collective action to fix the sector.
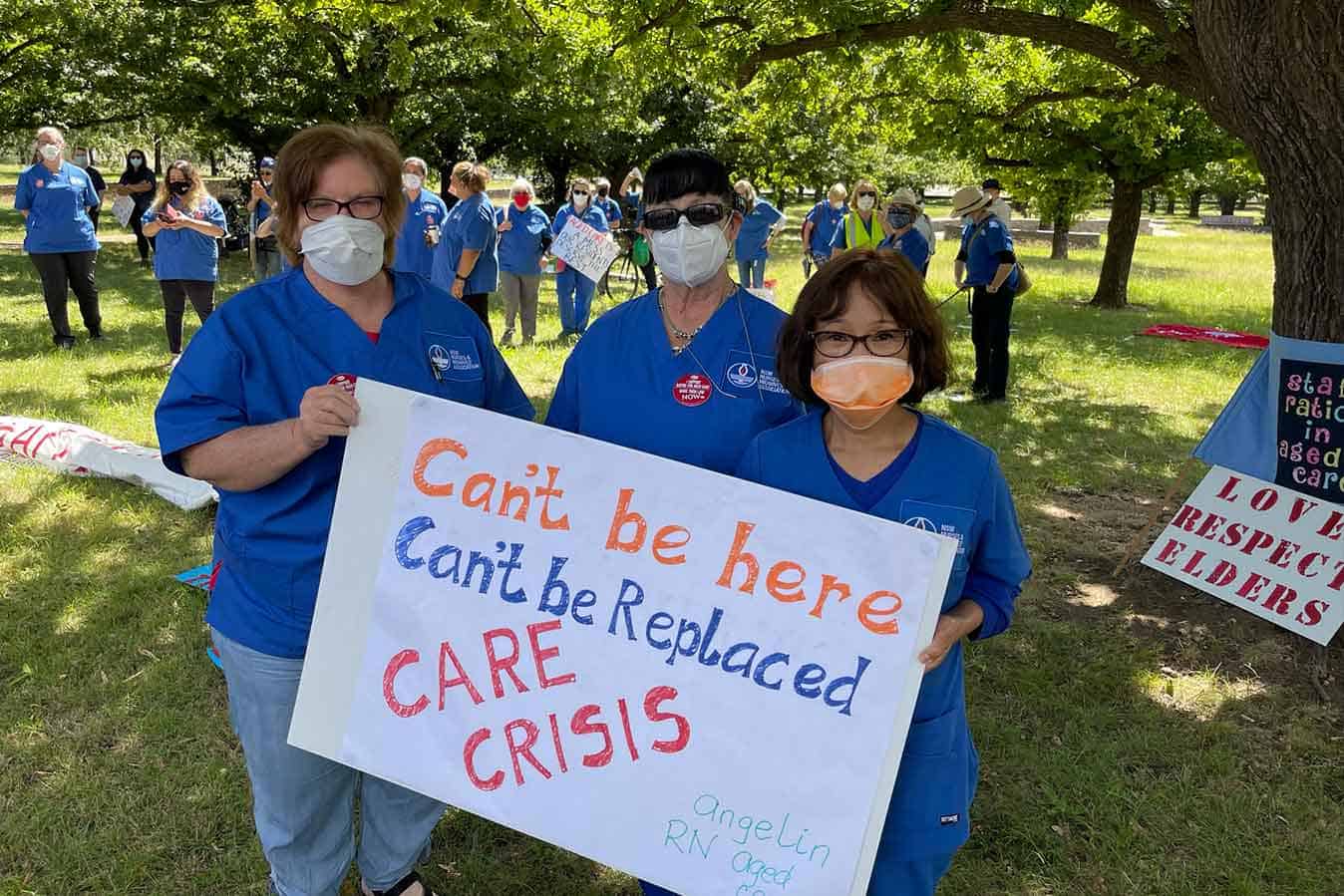
In early February, she joined aged care nurses and workers who travelled to Canberra to express their anger over the Morrison government’s ongoing failure to protect staff and residents during the current COVID-19 pandemic surge.
“I’d like to tell Mr Morrison everything is not alright. We were treading water before [the pandemic] but we’re actually drowning now. We can’t go any worse than what we are, we are in crisis, we’ve been in crisis a long time,” she said when speaking at the rally.”
Despite the uphill battle, Susan has no plans to leave the sector and is in for the long haul. For real change to occur, she believes that all Australians must speak up and join the cause in the lead up to this year’s federal election.
“The only way we will change aged care for everybody is if all Australians speak up,” she told the ANMJ.
“We’re all struggling and it’s just not good enough. “I knows it’s extremely difficult. I know a lot of people have left. I know our wage isn’t great and I know that we’re there because we care. We’ve been climbing up this mountain for a long time – don’t give up because we will continue to climb and we will get change.”








2 Responses
I left after 6 years of being a AIN . Only 2 care staff at times for 26 high care residents. That’s ridiculous. A lot of new staff were not trained properly and some couldn’t even speak, read or write English properly. The residents are suffering.
Hit the nail right on the head. I too work in aged care, in a 119 bed facility of one of the big aged care companies. I work nights in the dementia unit, which has 20 beds. I am there at night by myself. We have 1 RN at night, one PSW per section (there are 4) and 1 floater. Staff are overworked, underpaid and these companies are bringing in millions of $$ profit each year. The big wigs that run the show give their facilities meagre budgets. Staff are doing their best to attend to residents but staffing is not adequate.
It sickens me that the owners of these companies make huge profits every year, yet when we ask for more staff, their reply is “no money in the budget”. Things really should go back to PRE Howard Government when the companies had to account for their $$. These companies need to put their clients first, because if it wasn’t for them, they wouldn’t be making all the money they do.
Our facility is always running short staffed. Staff have done double shifts, stayed back to help out at times (not paid for it), and not being able to have their full 30 minute lunch break because they’re needed on the floor. It really is getting beyond a joke. This system is drastically broken and needs urgent attention. No one wants to work in aged care anymore because of the low staffing, workloads, low pay and stress from it all.