“Entering my patient’s room was something I’d done many times before but this time it felt slightly surreal,” says intensive care nurse Stephanie Lee of treating her first COVID-19 case on Good Friday.
“I walked in and introduced myself to my patient. After that, it felt like any other shift. My job was to care for my patient and try and make them feel more at ease in their time of need.”
Stephanie works in the Intensive Care Unit (ICU) at Tasmania’s Launceston General Hospital (LGH).
The global COVID-19 pandemic has penetrated Australia’s states and territories to different degrees. At the time of writing, Tasmania had more than 160 cases; exacerbated by a recent outbreak in the state’s north-west.
“It’s surreal because you are watching it unfold in other countries, and thinking ‘Wow’. And not just in third-world countries, it’s [overwhelming] developed countries with great healthcare systems [too].”
Stephanie admits feeling a little unnerved when she arrived on shift and was told she would be caring for a confirmed COVID-19 case, the first escalated to the hospital’s ICU.
She headed back to the change rooms and prepared to put on personal protective equipment (PPE) by removing her makeup, as it stains goggles and prevents a solid seal. The full PPE kit comprises hospital scrubs, a yellow gown, a white apron, two pairs of gloves, an N95 mask, goggles, a hairnet and rubber boots with shoe covers.
“Although I went about receiving handover for my patient as normal, there was a feeling of preparedness from all the staff around me,” Stephanie recalls.
“I would be working inside the negative pressure room with the patient and one of my fellow nurses would be working outside the room.
“It definitely made the pandemic feel much more real. We had been preparing and training for weeks, but now it was right here in front of me.”
Stephanie soon settled into the routine of a typical shift, caring for the patient and assessing vital signs. She lists having to use whiteboards and an intercom to communicate with colleagues outside of the room, and wearing PPE for long stints as the most challenging parts.
“The longest stretch I did in full PPE was three hours and it definitely takes a toll on you. You’re breathing becomes laboured and you aren’t able to touch your face to readjust your mask or goggles. By the end of my shift I had indents all over my face.”
Tackling the global COVID-19 pandemic
Like many hospitals around the country, LGH has been priming itself for a potential influx of patients infected with the virus.
It has a COVID-19 screening clinic outside the hospital and a dedicated COVID-19 ward to care for patients with the virus who do not require intensive care and the help of a ventilator to breathe. High-risk patients who present to the Emergency Department are being immediately screened.
In response to the crisis, the ICU has split up its operation between critically ill COVID-19 patients and those requiring general care.
At this stage, the LGH has dealt with relatively few COVID-19 cases and its efforts are focused on putting the correct procedures in place, minimising staff risk of exposure to the infection and making sure healthcare is delivered as seamlessly as possible.
As a frontline nurse, Stephanie now wears normal clothes when heading to work before getting changed there into her uniform, a gown, gloves and face shield.
Like many of her colleagues she has bought additional footwear made of rubber that can be wiped down and cleaned, which they leave at work after finishing a shift. Uniforms are laundered in hot water, with Stephanie showering before leaving work and again after arriving home.
“I’m lucky that I actually live alone so I don’t have to worry about bringing it home to other family members at the moment,” Stephanie says.
“But I’m definitely social distancing from the rest of my family. I actually just spoke to my grandmother on the phone and explained to her, because she doesn’t speak good English, that I can’t come visit for an indefinite amount of time until we don’t have these patient groups. It’s just taking those extra precautions to make sure we’re keeping everyone around us safe.”
PPE shortages
For nurses, the lack of protective equipment in the fight against COVID-19 has emerged as a major issue across the country.
Last month, the ANMF (Tas Branch) said nurses, midwives and carers across the state’s hospitals, general practice’s and aged care facilities were reporting shortages of PPE; prompting the union to call on state and federal governments to provide detailed information on stockpiles.
State Secretary Emily Shepherd has since told members that the union’s calls for additional PPE triggered a commitment from the state government that it will oversee its delivery to ensure it reaches areas in most need, along with assurances from health authorities that such equipment should not be reused, and only be used in line with Australian guidelines.

Stephanie says management at LGH have been upfront about available supplies, and that stocks are stable.
But she acknowledges seeing PPE shortages around the world was scaring many members of her profession.
“I’m not scared that I’ll contract COVID-19,” she says.
“I’m just worried that I would potentially pass it on to someone else who is more vulnerable in the community, or in the hospital. For me, it’s just being hypervigilant about what it is that I’m doing when I’m at work and out of work.”
“I think it’s something that’s really scary for nurses in general. We are always there to care for our patients as much as we can, but we’ve always had that safety net there of knowing that we have access to what seems like an unlimited supply of PPE so for people to have that feeling [of not having enough] I think it’s really hard for us as a profession to be able to deal with that. I know our workplace is working really hard to make sure we have enough supply of everything we need now and will also need going forward.”
Spotlight on intensive care
Intensive care units are staffed by teams of highly-trained clinicians, as patients require complex treatment to survive.
Caring for critical COVID-19 patients experiencing respiratory failure involves intubation, where nurses and doctors administer sedation before inserting a breathing tube into the airways that’s hooked up to a ventilator that pumps air into the patient’s lungs to keep them alive.

“We deal with death and dying on a daily basis in our workplace so it’s not something that’s new to us,” Stephanie says of the current situation in Australia, where at the time of writing there was more than 6,400 confirmed cases and 63 deaths.
“But obviously any person who comes in with something that’s potentially reversible, that we can help them with, we’re always going to do everything we can to help that person. So (whether it’s a COVID-19 patient or any patient) we always have that sadness when we haven’t been able to help that particular person.”
Stephanie says the delivery of healthcare in the face of COVID-19 is much the same but nurses and hospital staff remain on high-alert.
One noticeable difference is the empty corridors and lack of hustle and bustle since the hospital enforced visitor restrictions, but Stephanie believes the biggest change since COVID-19 is a newfound recognition for the profession.
“My job probably hasn’t changed, but people’s awareness of what I do has changed. I’ve had so many more people reaching out to me and checking in with how I’m going. As a nurse, that’s not something that we’re really used to; we’re usually the one’s looking after people.”
Stephanie, who also works part-time as a lecturer at the University of Tasmania, says responding to the pandemic has been challenging, largely due to uncertainty surrounding the virus.
“It’s the unknown of not knowing what’s coming, for us as nurses, for management, for the hospital. We’re not sure what’s going to happen so all we can do is prepare for the worst and hope for the best. We’ve just got this waiting game now to see if we have prepared enough.”
Containing the spread of the virus
In the past week, Tasmania’s COVID-19 numbers soared past 160 cases following outbreaks at the North West Regional Hospital and North West Private Hospital, which have since been closed to contain the spread. About half of the state’s COVID-19 cases are linked to this outbreak.
As a result, more than 1,000 healthcare workers as well as members of their households (estimated to total around 5,000 people) have now been placed into quarantine for the next two weeks. Fifty members of the Australian Defence Force and seven members of Australian Medical Assistance Teams were called in to assist the health system.
Stephanie says the rise in cases reinforces the need for health services and communities to follow precautions.
“It highlights how careful we need to be as healthcare professionals when we’re caring for patients that we know are confirmed cases because we don’t really know enough about the disease yet to know all the precautions that we need to be taking. We only have the beginning evidence of what’s come out of other countries.”
As part of the federal government’s plans to fight COVID-19, it recently announced free online training for 20,000 registered nurses to upskill in intensive care work and support the workforce if demand escalates, a move Stephanie welcomes.
“ICU is a really highly trained area and people who come to work with us do require a certain level of training and on the job training as well,” she explains.
“But I think it’s really positive in the sense that if we ever did come to a stage where we are so short of staff that we need other people, that those people are then going to be prepared. So they’re going to have some background knowledge to be able to assist us.”
Working together to keep each other safe
While Stephanie’s job is to look after critically ill patients, she is equally mindful of looking after herself and her mental wellbeing during COVID-19. She hasn’t accessed any formal support services as yet, but says many nurses are doing it tough.
“There are nurses out there that are scared. We all have fears about what’s going on and I would just say to them to reach out to their colleagues, their managers, anyone who they need to talk to, to actually discuss it and move on as much as they can, because if you hold all that fear in, I think that’s when we start to have a workforce that is too scared to look after patients potentially,” she says.
“I’ve just been taking time out for myself, shutting off social media for a little bit and just taking time to do those things for yourself like have a cup of tea, read book, and sit outside in the sunshine. We can’t go out into the community but we can do things at home that lift our spirits.”
Stephanie says community-led campaigns such as ‘Adopt a Healthcare Worker’ have been heartening for nurses and healthcare staff.
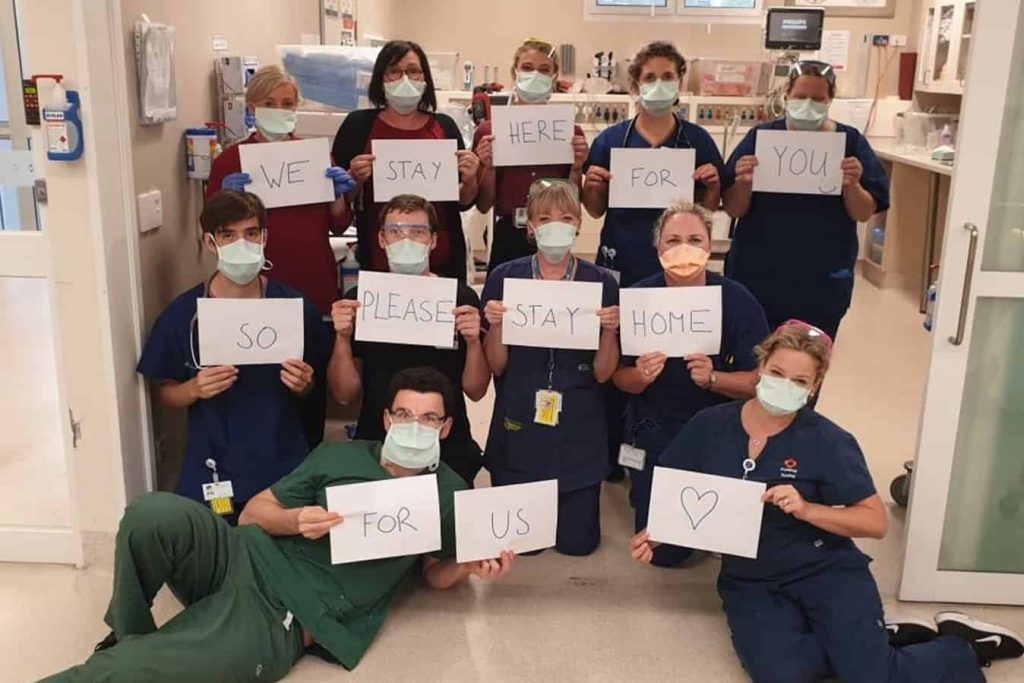
“Yesterday we actually had one of our local schools drop off some letters and a little care package for ICU and all the nurses and doctors, just saying how proud they are of us and how they appreciate everything that we’re doing, which I know touched a lot of people’s hearts. Even our coffee shop across the road from the hospital, people have been shouting a coffee for a healthcare worker when they come in. You don’t need those things but it’s just really nice to know that there is community support for us at the moment.”
As the pandemic’s peak looms closer, Stephanie says the workforce is galvanised and that a great camaraderie is being built among staff as they protect and care for patients.
“We’re just going to take it one day at a time. I’m really confident that we have an awesome team, and being in intensive care we rely on each other really heavily anyway, so we’re ready for whatever the external world is going to throw at us and at least we know we’ve got each other’s backs, whatever it is that does come.”








