Nurse practitioners and doctors are being enticed into working in rural and remote Australia by having their HECs/HELP debt entirely wiped, or slashed.
The new legislation, Higher Education Support Amendment (2022 Measures No.1) Bill 2022, introduced into Parliament today by the Federal Government, is aiming to encourage initial employment and retention of health practitioners to work in rural, remote or very remote areas of the country, to help address issues of equity and access to healthcare in these communities.
Under the program, a nurse practitioner or doctor who lives and works in:
- A remote or very remote town for a period of half the length of their course will have their entire HELP debt wiped.
- A large, medium or small rural town for a period equal to the whole length of their course will have their entire HELP debt wiped.
- An eligible place for a period of time equivalent to half the time required will be eligible to half the applicable debt reduction.
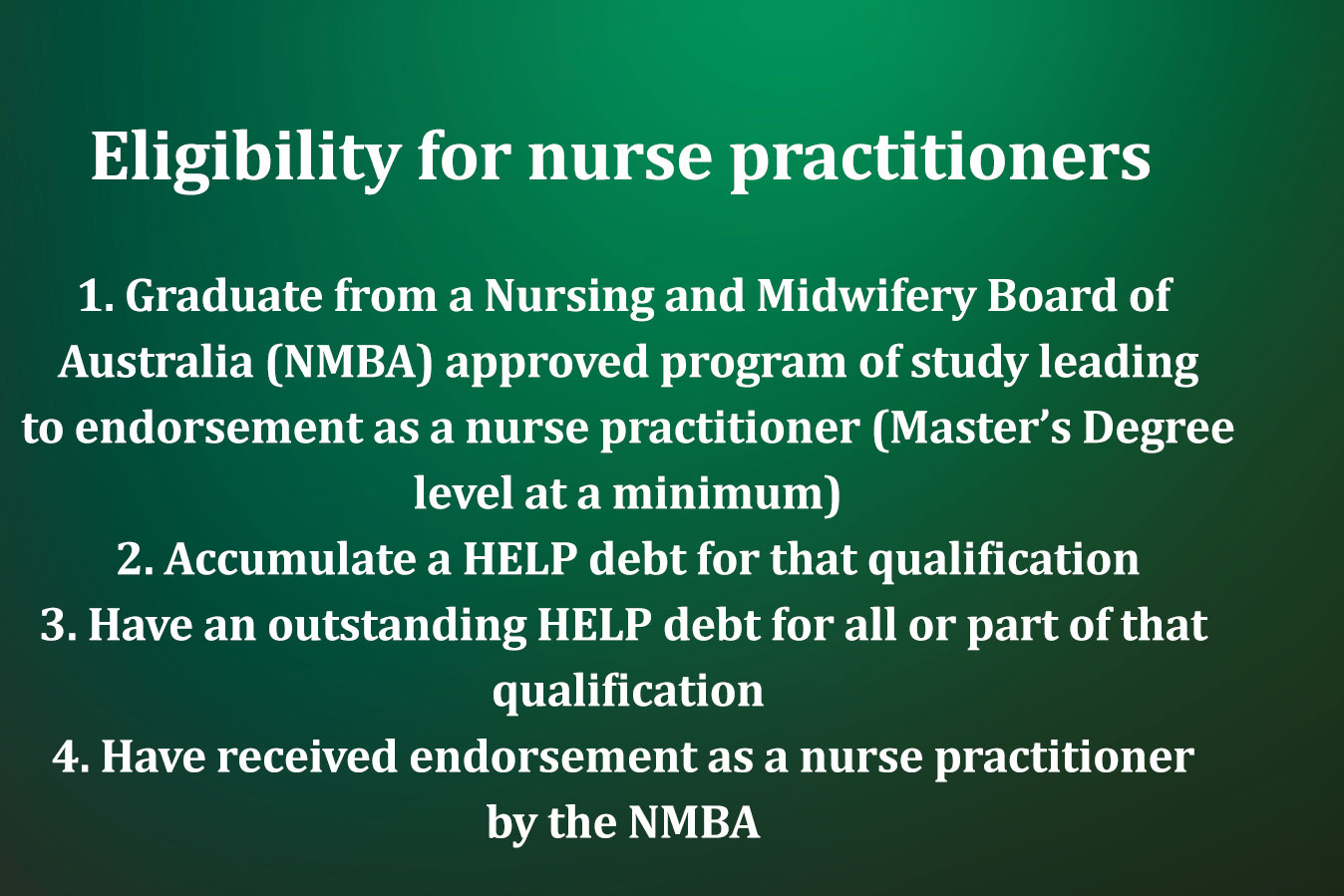
For nurse practitioners, the legislation will go towards covering a Master’s Degree in Commonwealth supported study, a full fee-paying place, or a combination of both.
If passed, the Government expects the legislation will help attract about 850 doctors and nurse practitioners each year.
The Australian College of Nurse Practitioners (ACNP), which contributed to the consultation process regarding the program, has welcomed the push to boost the number of nurse practitioners working in rural and remote areas.

Speaking to the ANMJ, ACNP President Leanne Boase said she believes the program will have a two-pronged effect, encouraging some people to consider moving out to rural and remote, while also helping to develop the existing workforce’s knowledge and skills.
“It will help bring people out to rural and remote areas but what’s really important here too is that it gives local health professionals already working a better opportunity to expand on their current education and knowledge or go into education in an area they want to work in and then stay in their local environment,” Ms Boase said.
“For instance, a nurse that’s working in a rural or remote area can now say ‘ok in order to provide more services for my local community, I’ve got support to go off and do this course’. In the past, that was just another hurdle for them. They’d end up relocating to the city, and stay there. So it will help to keep some of the most advanced nurses in those communities, train them up to work in those communities, and that’s where I see the biggest benefit of this.”
During the drat process, the College expressed significant concern over the program’s eligibility requirements, Ms Boase revealed. Under the original scheme, nurse practitioners would have been required to work in either an accredited GP practice, or a hospital, to be eligible. It would have meant few nurse practitioners would qualify and that NPs working in their own clinics would miss out.
The Government appears to have listened to the feedback, saying stakeholder identified issues in relation to the eligibility requirements for health professionals delivering primary care services, including in relation to both setting the setting where services are delivered and the remuneration arrangements for nurse practitioners, have been addressed.
“These concerns have been addressed in the overall design of the program, whereby the Bill establishes the program, eligibility requirements for the target health practitioners and the nature of the work to be undertaken to achieve the benefits of the program and provides for secondary legislation – the HELP Debtor Guidelines (Health Practitioners) – to articulate the specifics of eligible participants, eligible locations, and eligible work, and other arrangements to support the administration of the program.”
According to Ms Boase, people living across rural and remote Australia are unfortunately often forced to travel far-and-wide to access healthcare.
In some communities, nurse practitioners provide all of the care, within their abilities, and then refer people off only when it’s required, she added.
“A nurse practitioner can look after a huge range of health concerns,” Ms Boase said.
“They’re also very focused on health education and prevention, which is even more crucial in areas where there’s a lack of health services available, so they can offer a huge amount to a rural and remote community.
“But there’s obviously still barriers to practice that need to be dealt with. The fact that nurse practitioners can’t refer to a lot of allied health professionals, the fact that nurse practitioners are underfunded, and all those things. But if they’re enabled to work to their full scope they can certainly bring a lot to a community.”
Health Minister Mark Butler said the program would ensure all Australians have access to quality healthcare, no matter where they live.
“We recognise the challenge of recruiting and retaining primary healthcare workers in rural and remote communities,” Mr Butler said.
“These measures will make country practice a more attractive long-term career option for doctors and nurse practitioners.”








