All nurses will have heard of the term ‘model of care’, and many will have used it, but what does the term mean?
Background
A model of care (MoC) is a framework for guiding how teams’ function and clinicians deliver care in different settings and contexts. The term ‘model of care’ is often used to refer to different ways of approaching nursing practice and thus has been applied across a variety of contexts. Despite the term’s importance and common usage, there is no universally agreed definition. While definitions have been proposed by groups such as the World Health Organization, government bodies, and literature syntheses—they often don’t describe all aspects of how clinicians go about providing care.1
While some historical nursing MoCs can be identified and explained (e.g., the Team Nursing Model which emerged in the 1950s as a response to nursing staff shortages and dissatisfaction expressed by patients and professionals alike with currently popular MoCs),2, 3 they lack standardisation and still don’t cover the extent and breadth of comprehensive care delivery.2, 4, 5 This makes it challenging to update or adapt them to contemporary practices. As nursing practice and patient needs have evolved over the years, the philosophies and strategies of many older models have become outdated. This highlights the need for a contemporary definition and framework for nursing MoCs to be designed.2, 4, 5
We set out to create a clear and practical definition and framework for nursing MoCs. The full paper is published in International Nursing Review and can be viewed here. Here, we outline the main components of how we have defined ‘model of care’, provide key considerations for the design and implementation of a MoC, and explain a worked example.
A workable definition of ‘model of care’
Taking inspiration from earlier definitions, a MoC can be generally defined as the overarching framework that details all aspects of care delivery, including organisational structures,1, 2, 6 methods for the delivery of care,1 and guiding principles.7 At its core, a MoC describes the way in which care is delivered within a specific context.
To contextualise the components of our MoC framework, we will illustrate each component alongside a practical example of a nurse-led care coordination service within a multidisciplinary clinic,[1] provided in the commentary boxes.
[1] Adapted with permission from: Davis KM., et al. Continuity of care for people with multimorbidity: the development of a model for a nurse-led care coordination service. Aust J Adv Nurs. 2020;37(4):7-19.
Key considerations
Before designing and implementing a MoC, two critical considerations must be addressed; i) the concept and purpose of the model, and ii) the context in which it will be implemented. These are interdependent; each influencing the other. For example, understanding the health needs of a certain community (the context) will shape the model’s objectives (the concept).
a. Concept: Who is this MoC designed for? This includes the patient groups, health needs, and current service gaps the model aims to address. A key consideration is: what does this model intend to achieve and why?
| Example: The MoC was designed for the Australian regulatory setting, mainly in response to resource shortages during and after the COVID-19 pandemic. Its goal was to ease pressure on the primary care sector and keep patients safe by keeping high-risk patients out of hospitals. This was done by providing access to the MoC which included a specialist service that collaborated with primary care and a multidisciplinary team. |
b. Context: What factors should be considered when implementing this MoC? This includes economic aspects (such as funding), the current regulatory environment (are the workers qualified to deliver this type of care?), and considerations for the local culture. The list of considerations under this domain will be highly influenced by where, and in what sort of environment, this model is applied. It is important to think about what the people within this context need and to tailor the MoC to address this.
| Example: The model was designed for the outpatient setting to enable continuity of healthcare for people with multimorbidity. Through nurse-led care coordination, the model aimed to facilitate well-co-ordinated transitional care between the secondary and primary healthcare settings; monitoring and managing care allowing patients to remain in their home and reducing the need for hospital admissions. |
Key domains
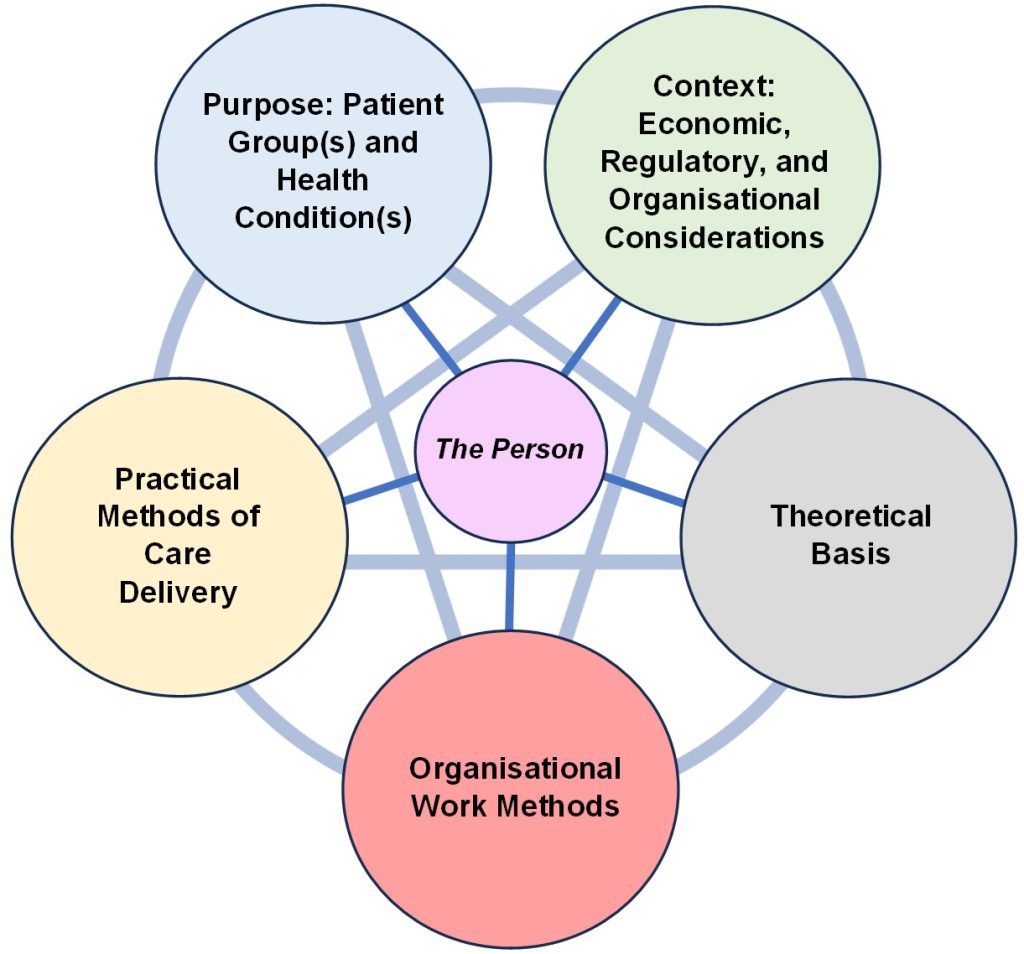
We proposed that a MoC involves three interrelated domains of 1) a theoretical basis, 2) organisational work methods, and 3) practical methods for care delivery. These domains are explained and presented alongside the example of a nurse-led care coordination service within a multidisciplinary clinic below.
1. A theoretical basis that guides how care is delivered and understood in all areas. Examples of a theoretical basis include ‘person-centred care’,8 ‘evidence-based care’,9 ‘holistic care’,10 and ‘value-based care’.11 Each of these provides a guiding principle for care, shaping all other aspects of the MoC.12 In choosing the theoretical basis(es), it is essential to address the most important aspects of care and determine how to best achieve this based on high level supporting evidence.
| Example: The theoretical basis of this model emphasised the delivery of person-centred, holistic, and individualised care within a nurse-led framework. In the context of this model ‘person-centred’ refers to an acknowledgment of the entirety of a person’s needs and preferences, beyond only the clinical or medical (i.e., holistic, individualised care), and allows for the concept of a person driving their own healthcare decisions in partnership with their healthcare team. Further, the model is evidence-based, incorporating tools and interventions supported by literature and resulting in the best outcomes for people with multimorbidity. |
2. Organisational work methods describe how people go about their work and their role, and includes details on aspects such as clinical decision making, assessment, delegation of care responsibilities, organisational governance, and how to collaborate with other healthcare teams and the wider organisation.2 Broadly this domain describes the responsibilities of each member of the healthcare team.
| Example: The model was led by nurses who coordinate care within a multidisciplinary team. The nurse care coordinator ensured continuity of care, managed referrals, and engaged patients through ongoing assessments. Governance was based on shared responsibility, clear leadership, and engagement among professionals. Implementation will vary based on local resources and policies; however, the model required that a senior nurse always lead the clinical aspect of care delivery. |
3. Practical methods of care delivery (Care Processes) that ensure that the care provided aligns with the theoretical basis. For instance, while the technique for giving an injection may not directly reflect a patient-centred approach, the practitioner’s attitude does. They might use empathetic language, like describing the injection sensation as “pressure” instead of “sting,” to ease the patient’s discomfort. This domain may also address ‘who’ delivers care and ‘why.’ For example, in a person-centred MoC, a nurse might educate and supervise a patient with diabetes to self-administer insulin injections. This empowers the patient to take charge of their diabetes management, enhancing the safety of at-home injections and improving care outcomes. In other situations, for example, a patient with a needle phobia, an individualised and person-centred approach, informed by therapeutic evidence, would be employed instead. In this way we can see that care delivery in this example is driven by the decision-making framework described by the ‘organisational work methods’ domain that includes assessment, monitoring, and evaluation with consideration to the ‘theoretical basis’ of person-centred care. To this extent, it can be observed how all the domains complement to inform how care is practically delivered to meet the specific health needs of the population it serves.
| Example: The model upholds the theoretical basis of ‘person-centredness’ in practical terms through a comprehensive care planning process. This method of care delivery enabled patients to work collaboratively with clinicians to set individual clinical health goals, and discuss and make decisions regarding their unique physical, emotional, social, and spiritual needs. These might include considerations around perceived/experienced health and wellness, functional status, mental health/psychosomatic concerns, medications, family/caregiver situation, spirituality, and assessments relevant across the lifespan. Within care delivery, patients were consulted at all stages which allows for the building of trust and rapport and individual acknowledgment. |
Figure 1 displays a framework for how a MoC can be conceptualised and depicted, with each domain, and the key considerations influencing each other and ultimately impacting upon the care delivered to the person at the centre of the model.
Conclusion
We hope that this definition will serve as a resource for researchers, policymakers, and practitioners. It could be helpful in defining and explaining current MoCs and helping to pinpoint existing gaps in care delivery and areas needing improvement. The definition and framework could help nurses design innovative nursing models that reflect contemporary practice and address the evolving needs of patients in their own practice contexts. It can also serve as a tool for advocating for new models, ensuring that they receive the attention, support and funding necessary for successful implementation. We envision this definition as a catalyst for meaningful change in nursing practice, enabling professionals to enhance care quality, promote patient-centred approaches, and ultimately improve health outcomes across diverse populations.
References
1. Davidson P, Hickman L, Graham B, Halcomb E, Phillips J. Beyond the rhetoric: what do we mean by a ‘model of care’? Aust J Adv Nurs. 2006;23(3):47-55.
2. Parreira P, Santos-Costa P, Neri M, Marques A, Queirós P, Salgueiro-Oliveira A. Work Methods for Nursing Care Delivery. Int J Environ Res Public Health. 2021;18(4).
3. Fairbrother G, Chiarella M, Braithwaite J. Models of care choices in today’s nursing workplace: where does team nursing sit? Aust Health Rev. 2015;39(5):489-93.
4. Hughes R. Patient safety and quality: An evidence-based handbook for nurses. 2008.
5. Duffield C, Roche M, Diers D, Catling-Paull C, Blay N. Staffing, skill mix and the model of care. J Clin Nurs. 2010;19(15-16):2242-51.
6. Splaine Wiggins M. The partnership care delivery model: an examination of the core concept and the need for a new model of care. J Nurs Manag. 2008;16(5):629-38.
7. Innovation AfC. Understanding the process to develop a Model of Care: An ACI Framework. Chatswood; 2013.
8. American Geriatrics Society Expert Panel on Person-Centered Care. Person-centered care: a definition and essential elements. J Am Geriatr Soc. 2016;64(1):15-8.
9. Rycroft-Malone J, Seers K, Titchen A, Harvey G, Kitson A, McCormack B. What counts as evidence in evidence-based practice? J Adv Nurs. 2004;47(1):81-90.
10. Jasemi M, Valizadeh L, Zamanzadeh V, Keogh B. A concept analysis of holistic care by hybrid model. Indian J Palliat Care. 2017;23(1):71-80.
11. Tseng EK, Hicks LK. Value based care and patient-centered care: divergent or complementary? Curr Hematol Malig Rep. 2016;11(4):303-10.
12. McEwen M. Overview of theory in nursing. Theoretical basis for nursing. 2014:23-48.
Authors
Jarrod Clarke is a Research Assistant in the ANMF National Policy Research Unit (Federal Office) based in the Rosemary Bryant AO Research Centre, Clinical and Health Sciences, University of South Australia.
Dr Kate Davis is a Research Associate at Rosemary Bryant AO Research Centre, UniSA Clinical & Health Sciences, University of South Australia.
Dr Jane Douglas is a Professional Officer and the Strategic Lead for Workforce at the Australian Nursing and Midwifery Federation (Federal Office)
Associate Professor Dr Micah DJ Peters is based in the ANMF National Policy Research Unit (Federal Office) in the Rosemary Bryant AO Research Centre, UniSA Clinical & Health Sciences, University of South Australia.








