A Queensland rural and remote nurse is undertaking research to help establish the essential skills required for all nurses new to rural and remote to help in their preparedness, along with support.
“I’m hoping the research will support new RNs to stay. A lot of metropolitan nurses, post Covid have decided to get out of the city. I want to also focus on those experienced nurses who need support, education and mentorship as well. They are experts at oncology or renal or medical, whatever field they’ve worked in, but they’re new to rural and remote,” said CQUniversity PhD candidate Danielle Rogers.
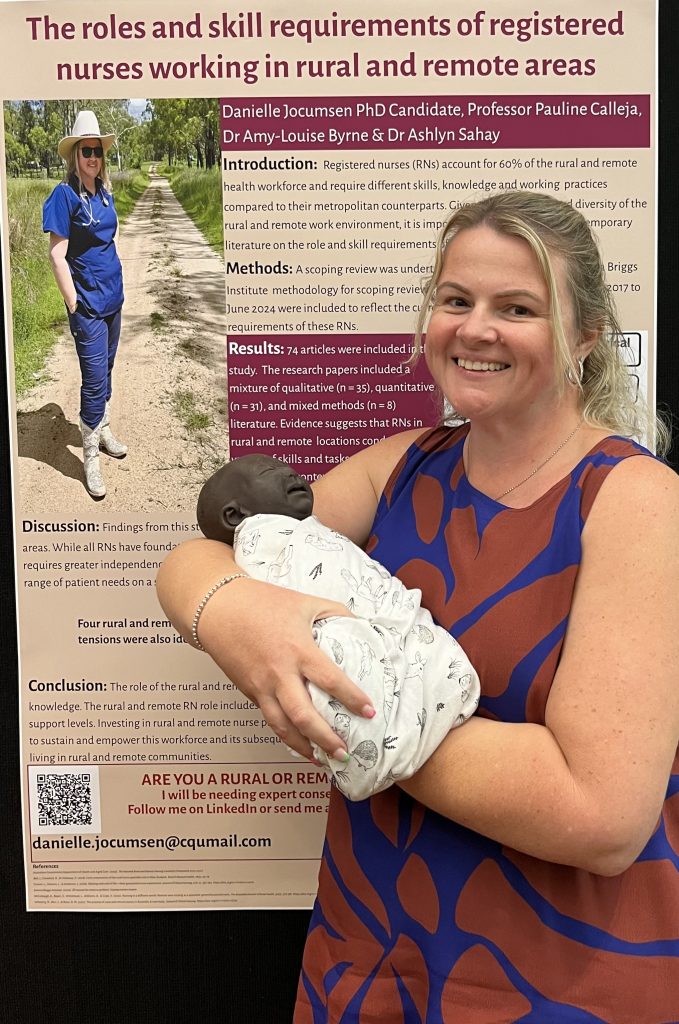
Phase one of the research was a scoping review on the roles and skill requirements of rural and remote registered nurses which has just been accepted for publication in the Journal of Clinical Nursing. Phase two involved qualitative interviews with 24 participants in two cohorts: new RNs going rural and remote, and experienced RNs.
“I wanted to hear about their experiences, their preparedness and, and everything about going rural and remote. What we found is that it takes more than preparedness, they need support,” said Mrs Rogers.
Invaluable experience and life skills
Mrs Rogers spent three years working as a remote nurse, completing her Rural and Isolated Practice Registered Nurse (RIPRN) and Immunisation Endorsement.
“I don’t think I would be the nurse I am today if I didn’t go out there. I learnt so much more than if I stayed at a regional or a metro hospital. I was triaging eight weeks in; I tube-assisted my first patient in about my third week. At the time it was a little overwhelming because everything was just happening.
“I remember one night a farmer had a tendon injury in his leg. He was adamant that he was not being flown out because he had a farm to attend to and there was nobody else that could do it. This man needed this tendon repair, and he was just, ‘I’m not going’. So, the doctor said to me, ‘let’s repair this tendon’.
“I had one general surgery kit, and we repaired this tendon. If I was working at a regional or a metro hospital, I would never have the opportunity to do any of that.”

She often draws back on her knowledge and the advanced skills she gained from her experience working remote, and sometimes the transition back can be challenging.
“Obviously you can’t repair a tendon when you come back, but there’s other things that you’re restricted in doing. I was able to dispense antibiotics, and I could give S8 drugs as per the drug therapy protocol. I came back and I couldn’t even do nurse-initiated paracetamol because I hadn’t done the package and yet I’m a RIPRN nurse.”
Context focused training
One of the challenges mentioned by several participants during the research was the lack of rural and remote focused training, said Mrs Rogers
“A group of grad nurses went to do advanced life support at a regional facility training. They were working in a team of eight during a met call. One of these grads put a hand up and said: ‘I work in a rural facility, and it’ll be me and an enrolled nurse. What do I do?
“In here, we hit a button, and everyone comes – someone is the scribe, someone’s on drugs, someone’s on the airway, the runner, the timer, whoever. I need to get my head around when there’s just two of us. How does this work?’ And they just kept saying to her: ‘this is not what we’re doing today.’ And this poor grad nurse is asking: ‘why am I here?’
“Yes, you’ve got to have advanced life support, but the content needs to be context focused because our new nurses are struggling with courses that are run in regional and metropolitan facilities and then trying to adapt it back to their rural or remote facility.”
Rural communities
Some of the challenges is adjusting to living in rural communities, not rural and remote nursing itself, says Mrs Rogers.
“When you go out in the community, you’re professional all the time because there’s no place that you’re probably not going to be seen, and word gets around.
“If I was working a late shift and I had to go grocery shopping, I had to make sure I was in there by about 9am when the shops opened because there was no way I was coming home by 12 noon.
“I don’t mind chatting to people, but the grocery shop would take a good couple of hours because every time you’d turn the aisle, you’d see someone else that would have a chat. I couldn’t go shopping an hour before my late shift because there was no way I was going to make it there.”
Minimum skill set
The next phase of the study, which is an expert consensus round, will focus on what is the minimum support requirement for nurses going rural and remote, aimed to be completed by mid-year.
“It’s going to be an expert consensus on what is essential skills and what is ‘nice to have’ skills. Breaking it down to essential skills and beneficial skills in a rural facility, and essential skills and ‘nice to have’ type skills in a remote facility.
“Once we’ve got that information, we will look at what can we do to support these nurses? What positive supportive environments do we need to encourage nurses to work in rural and remote, not necessarily to stay, because I think we’re moving into a workforce where people like to move around.
“But even though nurses leave a facility, sometimes they go back to rural and remote. But if they haven’t had that good experience and that good support, they’re not going to go back.”
Go rural
If you’re thinking about going rural and remote, do it, says Danielle. “I think that everyone should have a go at rural and remote. I always tell my students, ‘If you can do it, then do it.’
“I’ve been sharing my experience with my students, so they get an idea of what it’s like. What should you consider and what are some of the things you’ll expect? I think if you’ve got that preparedness, you’ve got that mindset, you can do it.
“Even if it’s just one of your nursing placements, or your graduate year. If you don’t like it, you don’t have to stay. And it’s ok if you don’t stay, but you can always go back.”

Bonds
Mrs Rogers plans to go back to remote with her family once she’s finished her PhD. She calls the Queensland town of Monto where she went as a graduate her second home.
“I loved it out there. I loved the community. I lived with the cook’s mum, and I call her grandma still. She’s 96 and I go out and see her every year. I got married two years ago, and she came to my wedding.
“You make these bonds when you go out there. Harvey Bay is home to me because that’s where my family is. But even though I left Monto in 2012, it’s still home to me.
“We go and visit everyone. When some of the staff come to Harvey Bay, I catch up with them for coffee. It’s not just about the rural and remote work; it’s about the community.”
During her time in Monto, there was a flood, which included the evacuation of people who were stranded. “I did extra shifts and the grass in my yard, once the water had subsided was up to my knees. I didn’t have time to mow with all these extra shifts I was doing. I came home one day from work, and somebody had mowed my yard. To this day I have no idea who did it.”
Making a difference
Mrs Rogers hopes her research will help make positive impact on the nursing workforce.
“But I also want to make sure that people living in those areas have the best care. We know sometimes it’s so hard to deliver care to these people, whether it be they can’t get somewhere, or they just don’t want to go. And that’s ok as well.
“They don’t want to leave their farm, or their community, to get healthcare. The more support we can give to the workforce, the better care we can provide these people.”
Danielle Jocumsen (Rogers) was featured on the ‘A Nurse Out Where’ rural and remote podcast series by rural and remote nurse Danielle Causer. Listen to the podcast here: Episode 81: What are the needs – A Nurse Out Where – Apple Podcasts









One Response
What you have said is very true. I work rural and in an emergency there may be only 2 of you until extra help comes. I started rural nearly 47yrs ago and we could do a lot more and GP’s could do a lot more procedures than they do now for many reasons. I still prefer rural over metro or city and enjoy carering for my community