The risk of hypothermia when transfusing during trauma situations could be prevented thanks to a simple, one-piece, disposable latent heat fluid warmer developed by Flinders University researchers in South Australia.
When blood is required for major trauma outside of a medical facility, the risk of hypothermia increases when a patient is transfused bags of blood taken directly from chilled storage.
The warmer provides a safe solution to overcome this problem, the university said.
“Major trauma is associated with blood loss and hypothermia. It’s common to replace lost fluid with red cells stored at 2-6 degrees Celcius, and colloid/crystalloid fluid stored at ambient temperature, thus increasing hypothermia risk,” said lead researcher Dr David Roxby.
The difficulty warming blood at trauma and medical retrieval sites is that mains electricity-powered fluid warmers cannot be generally used.
However, using latent heat, powered by solidifying calcium nitrate tetrahydrate, from fluid warmers raised the temperature of the red cell units to approximately 35°C, which therefore provided an alternate practical and efficient method of portable temperature‐controlled intravenous fluid warming, the researchers said.
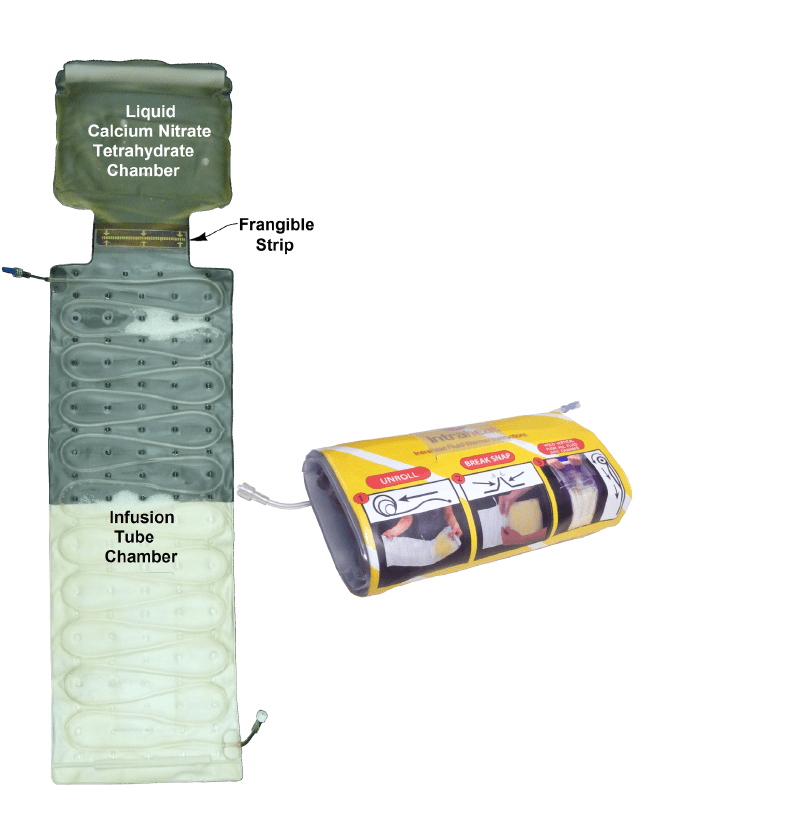
“The great advantage is that latent heat can warm fluid to normal body temperature without electricity,” Dr Roxby said.
“This study proves that a portable latent heat fluid warmer – which weighs only two kilograms and warms up in less than one minute – is safe to use and does not overheat.”
Currently, intravenous fluid warming for emergencies in remote locations occurs via a range of methods which have limitations and even potential dangers. Using warm water to heat fluid bags may take too long to reach the required temperature and carries a risk of bacterial contamination. Electric warmers often need external batteries that take vital time to assemble and need to be kept charged. Some chemical reactions can heat fluid above normal body temperature, potentially damaging the blood product.
Using the latent heat fluid warmers that increased the temperature of red cell units to approximately 35°C, showed that there were no significant differences in haemolysis markers (plasma haemoglobin, potassium, lactate dehydrogenase, bilirubin) following warmed and unwarmed transfusions.
Videos, showing latent heat fluid warmers operating, can be seen at: http://intraheat.com.au/
The paper – Warming blood prior to transfusion using latent heat was published in Emergency Medicine Australasia. (https://doi.org/10.1111/1742-6723.13471)








