A new national framework has been released to support health services to reduce medication-related errors and hospital readmission rates for patients who are transitioning between care settings.
The Australian Commission on Safety and Quality in Health Care’s Medication Management at Transitions of Care Stewardship Framework provides the first coordinated, hospital-based approach to manage medicines during this high-risk period for patients.
Transitions of care for patients who move between hospital and primary and aged care settings can pose challenges and risk of medication error, particularly for people with complex care needs.
More than 50% of medication errors occur at transitions of care. Each year in Australia, 250,000 hospital admissions are due to medication-related errors.
Identification of high-risk patients
One aim of the framework is to promote identification of patients at high risk for medication-related problems. This can include:
- people who are aged over 65 years,
- those who take five or more medications or take a high-risk medication, and
- those with multiple prescribers for their medication.
The framework articulates a stewardship model for these patients which includes comprehensive medication reconciliation, regular medication review and early discharge planning and liaison.
“We know that a lot of hospitals are very good at mitigating risk for medication error,” said Dr Phoebe Holdenson Kimura, Medical Advisor for the Commission and a general practitioner.
“The framework is designed to be incorporated into existing systems and clinical practice to enhance medication governance, improve communication, and facilitate timely, collaborative post-discharge medication review, especially for high-risk and vulnerable patients.”
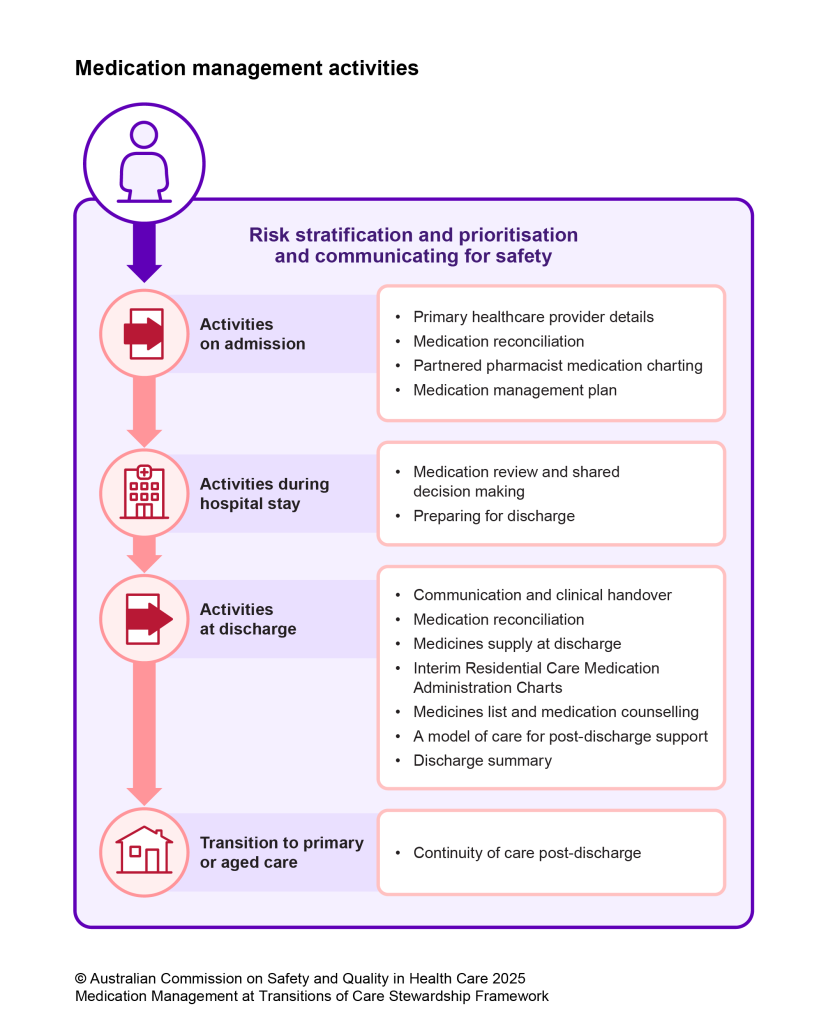
The framework supports emergency departments to identify people at high risk of medication-related problems and prioritise them for medication reviews throughout their hospital stay. The proactive approach is aimed to reduce medication error at admission, during a hospital stay and at discharge.
There is a real opportunity for hospital clinicians to adopt the new framework and take action to strengthen communication with the primary and aged care sectors, said Dr Holdenson Kimura.
“Individuals with one or more medicines missing from their discharge information are far more likely to be readmitted to hospital than those with correct information at discharge.”
Many clinicians had experienced first-hand the success of the antimicrobial stewardship model in hospitals, which supports the judicious use of antimicrobials, said Dr Holdenson Kimura.
“It would be fantastic to see the adoption and implementation of this medication management stewardship model embedded in Australian hospitals, similar to the antimicrobial and opioid stewardship models to improve patient care,” she said.
Digital tools are key to reach potential of the framework
Health services are encouraged to adopt safe, high-quality digital tools to strengthen communication between clinicians across settings and improve medication management at transitions of care.
“Digital enablement will be key to realising the full potential of the framework, but these digital tools need to be interoperable to enable accurate and timely communication,” said Dr Holdenson Kimura.

“Within the hospital setting, the digital system needs to be seamless and easily accessed by different members of the care team. This would mean that prescribing software and pharmacy dispensing software is working well together to support discharge.
“To streamline communication about medication use across settings, standardised electronic discharge summaries would be delivered automatically and securely at the time of discharge, and uploaded to the patient’s electronic health record, such as My Health Record.”
The framework was developed as part of the Commission’s leadership on Australia’s response to the World Health Organization Global Patient Safety Challenge: Medication without Harm. This challenge was focused on reducing severe, avoidable medication-related harm by 50% over the five years to 2024 with an emphasis on high-risk medicines, polypharmacy and transitions of care.
The Medication Management at Transitions of Care Stewardship Framework is available here








