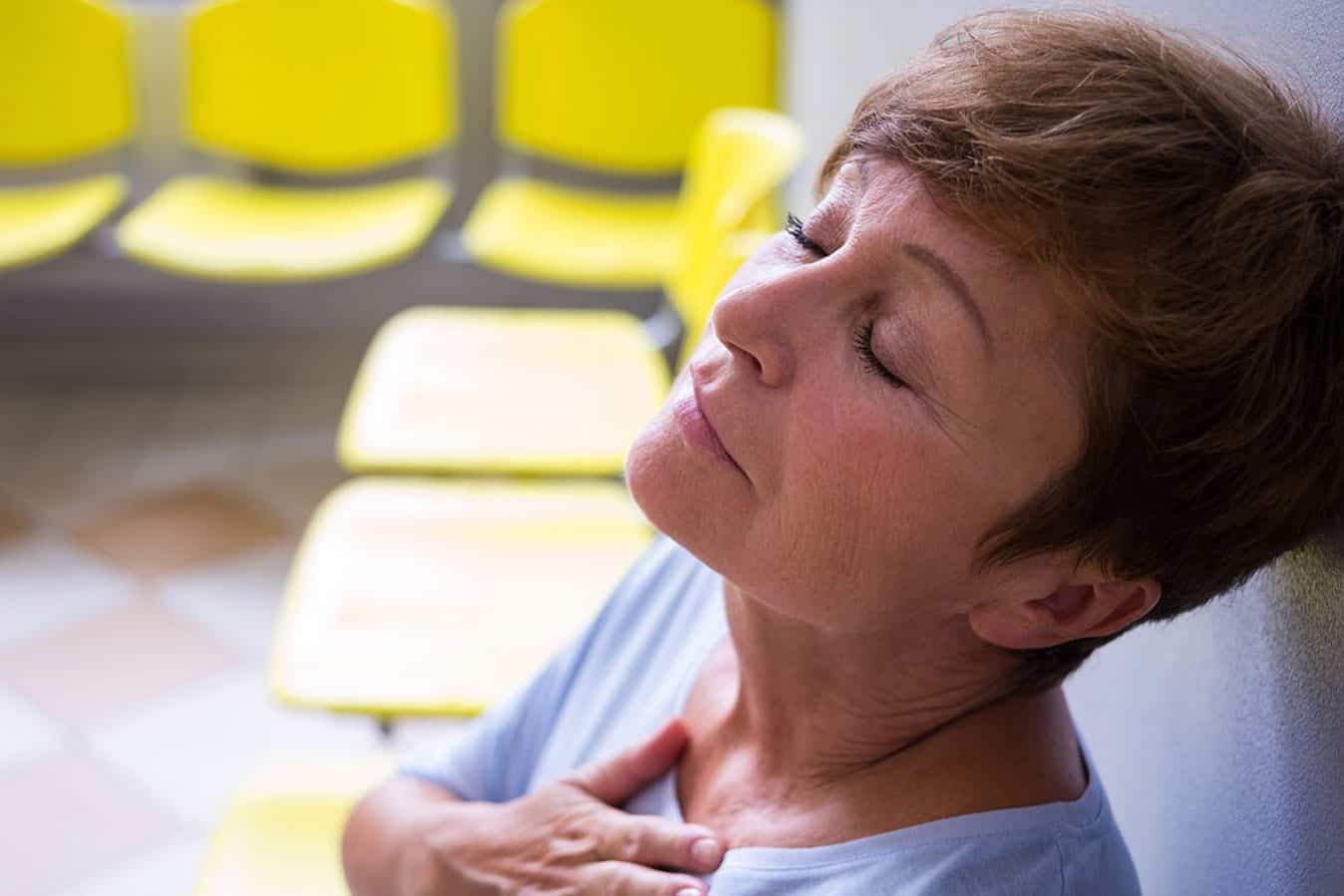
It is a scenario that is played out in emergency departments across Australia every day – a woman comes in with symptoms that don’t fit with the archetypal heart attack.
She is not complaining of severe chest pain or clutching her chest. Her symptoms of extreme fatigue and shortness of breath have been happening on and off for weeks and may mimic something else, so she slips down the queue.
Heart disease is the number one killer of women in Australia and across the world, but is not often given the attention it deserves. If a woman is having a heart attack (‘acute myocardial infarction’) she is more likely to have delayed treatment than men, increasing her risk of death.
This inequitable situation has been my major research focus for the past decade.
Back in 2007, I had a chance conversation with a colleague while working as an emergency nursing lecturer. She told me about research from the US highlighting the disparity between women and men who had heart attacks and I wondered if there were similar challenges in Australia.
I decided to do a PhD to look at the issue and found that in Australia, women were treated differently too.
Compared to men, women received delayed treatment, fewer tests, and less cardiac unit admissions. Women with some types of heart attacks were twice as likely to die in hospital than men.
This work shows a need to reappraise decision making by clinicians when assessing women for heart attacks and the processes involved in getting patients access to evidence-based care as quickly as possible. It demonstrates the need to raise awareness of possible gender differences in heart attack management.
My current work involves developing a predictive model to see which women do not receive evidence-based care so that this can be avoided. To do this, I’m looking at the role of numerous factors including symptoms, age, co-morbid illness, preferred language and socioeconomic status.
We have assumed for too long that heart disease in women and men are the same, but now we are starting to think that the conditions may differ between genders. One of the problems is that most of the research on heart attacks has been done on men. Even the diagnostic tools we use such as stress tests are based on research done mostly on men. The truth is that women are not simply smaller versions of men. Their blood vessels can react differently during a heart attack and the role of hormones and many other factors come into play. Diabetes and high blood pressure, including during pregnancy are important risk factors to consider when a woman presents for treatment.
There is still a long way to go, and much we don’t yet understand, but it is imperative that we don’t consign women to preventable early deaths or heart failure by not acting quickly enough to limit the damage done to their hearts.
Morbidity and mortality are avoidable, if clinicians apply the evidence to their practice.
Dr Lisa Kuhn is an emergency nurse and member of the Centre for Quality and Patient Safety Research (QPS) in Deakin’s School of Nursing and Midwifery.