A study investigating the links between sleep and pain could fundamentally change the way clinicians treat people with chronic pain.
National Health and Medical Research Council (NHMRC) investigator and pain scientist Dr David Klyne, of the University of Queensland, discusses his current research, which is looking into how sleep influences pain recovery.
What is your research about?
Poor sleep coexists with chronic pain in up to 90% of cases. But we don’t know if poor sleep actually drives chronic pain. This research will enable us to establish whether that’s the case. And that’s really important because if poor sleep does indeed have a contributing role to chronic pain development and maintenance, then we can start to look at treatments for sleep to better manage chronic pain.
Why is sleep important?
Sleep has an enormous impact on our immune system. It’s essential for a healthy immune system. Now, if that sleep is disrupted or it’s not as good as it could possibly be, that can have a trickledown effect on the immune system and result in excess inflammation within the body that can stimulate nerves and pathways that are involved in pain.
What is the relationship between sleep and pain?
For some time, we’ve known that sleep and pain are related. Our research, however, suggests that contrary to traditional belief is that sleep more likely influences pain than the other way around.
Worse sleep primes the nervous and immune systems to enhance pain and potentially drive the development of chronic pain. Whether or not you develop chronic pain might be dependent on how you’re sleeping at the time, during your acute pain period. It might actually have a causal role in the transition from acute to chronic pain.
How does chronic pain affect people?
The current definition of chronic pain is pain that persists or recurs for more than three months. This form of pain occurs in at least 20% of the world’s population. Put simply, it’s the biggest unresolved health challenge of our time, and it causes more disability than cancer and heart disease combined.
The economic and human costs are enormous. And the key nugget with sleep, if we identified it as an important factor, is that poor sleep coexists in up to 90% of people with chronic pain. That’s an awful lot of people.
Do we need to change how clinicians treat pain?
Sleep as a treatment for pain is largely overlooked. This work could really fundamentally shift how the health system considers sleep in the context of pain. If we can increase our understanding about the relationship between sleep and pain, we can hopefully encourage more clinicians to consider sleep as a legitimate treatment for patients with pain.
How will you conduct the study?
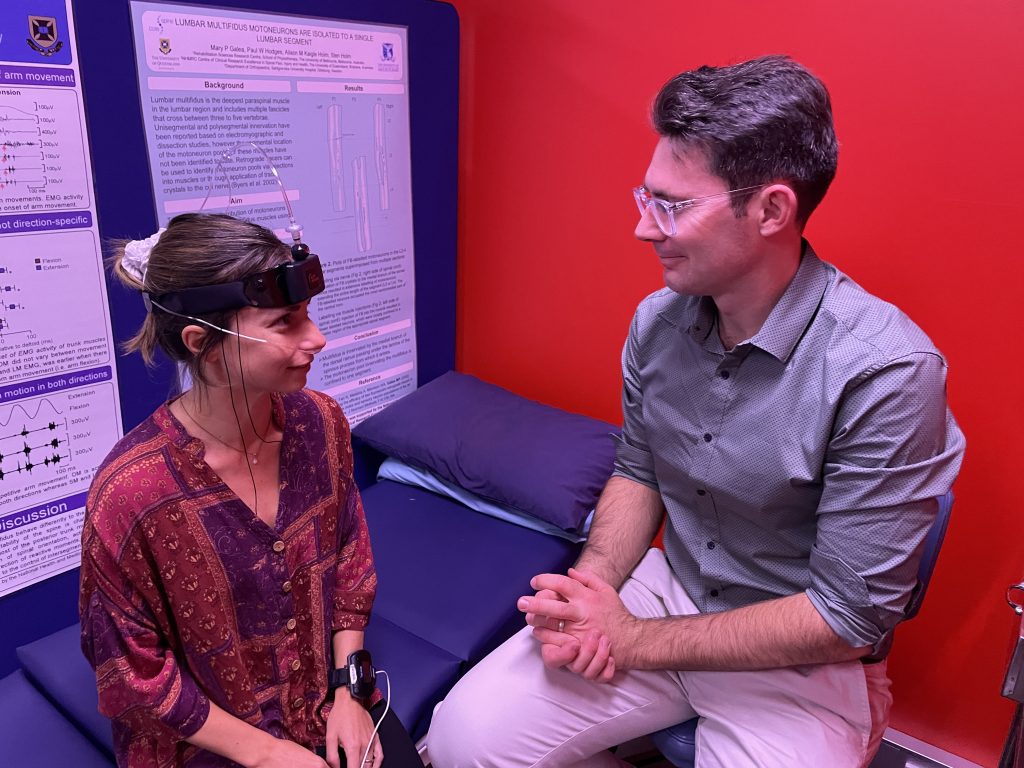
We’ll be bringing in about 50 participants who are experiencing chronic pain and measuring the brain activity using head devices to monitor their sleep patterns, while also conducting blood and saliva tests to look at hormonal, neural and immune responses. These measures will be collected over an eight-day period.
We’ll observe how their nervous and immune systems respond to a period of good sleep and a period of poor disrupted sleep, which will be achieved by participants setting alarms at intermittent times throughout the night.

We’ll also be examining if, and how, different sleep patterns – such as deep sleep and light sleep – impact recovery differently. For example, disrupted or loss of deep sleep might influence someone’s recovery far more than loss of light sleep.
How does this study fit into your other research?
This project is part of a bigger picture on how lifestyle factors influence pain. One of our projects, a US National Institutes of Health-funded study, is currently recruiting for a study to examine how back pain symptoms are influenced by biology, psychology, sociology, behaviour and lifestyle.
The research team is looking for participants aged 18 and older who have experienced back pain on at least two days in the past two weeks.
More information and registration to participate is available on the study volunteer page.









2 Responses
G’day
I have chronic pain from ESD and insomnia, for which I take melatonin, which works better than not taking it.
I have bad days for pain and some nights awful, but others OK.
I’m a Registered Nurse and work, part-time, as a Clinical Research Nurse in Oncology, at SCUH.
I live on the Sunshine Coast and happy to travel to Brisbane.
Hi Christine, more information can be found here – https://habs.uq.edu.au/back-pain