Australia has recently reached the end of the latest wave of COVID-19 infections that occurred over the winter months.
This wave of steadily increasing numbers of new and active COVID-19 cases from early June also resulted in a significant increase in the number of people in hospital, outbreaks and cases in nursing homes, and increased burden on intensive care units (ICUs) and healthcare staff more generally (See Figure 1).
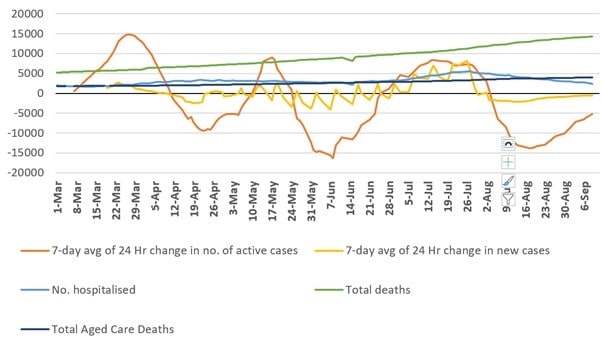
Figure 1: Active cases (7-day moving averages of daily change), new cases (7-day moving averages of daily change), number of people in hospital, and total deaths reported.
On the 14th of July the Deputy Chief Medical Officer Michael Kidd announced that this wave was caused by the BA.4 and BA.5 sub-variants of the Omicron SARS-CoV-2 variant. Of testing that was conducted in the three weeks prior to the 11th of July, 46.5% of cases were of the BA.5 strain, and only 38.8% of the previously dominant BA.2 strain. By the later half of July, the wave appeared to have begun to subside and by mid-August, case numbers and hospitalisation figures had returned to pre-wave levels.
Although evidence is still emerging, it is clear these new strains were able to more effectively evade existing vaccine immunity and immunity conferred by past infection. While highly transmissible, the sub-variants appear to have not been the cause of as much severe illness as previous variants based on only minor increases in ICU admissions and ventilator use, however the wave did still result in peaks in hospital use and COVID-19-related deaths (See Figure 2).
Figure 2: 7-day moving averages of daily changes in hospitalisations, ICU admissions, people on ventilators, and deaths.
What are variants?
As viruses mutate and evolve, new variants of the original ‘index virus’ emerge that have different genetic features and can behave differently such as by becoming more highly infectious due to changes in the spike proteins that allow the virus to infect human cells, or less likely to cause severe illness due to a greater propensity for colonising the upper respiratory tract rather than the lower airways.1
‘Variants of concern’ are those that have; i) increased transmissibility or cause a detrimental change in COVID-19 epidemiology, or ii) increased virulence or changed clinical disease presentation, or iii) caused a decrease in the effectiveness of public health and social measures or available diagnostics, vaccines, or therapeutics.2
So far, there have been several variants of concern including, most recently, the Delta and Omicron variants. Sub-variants can also be of concern. Sub-variants are of concern if they belong to an already circulating variant of concern (e.g., Omicron) and show signs of transmission advantages compared to other circulating variant of concern linages as well as amino acid changes that are known or suspected to result in changes to the epidemiology and fitness advantages. There are several sub-variants of the Omicron variant including BA.4, BA.5, BA.2.12.1, and BA.2.75. As new evidence emerges, it is possible that a sub-variant of concern might be found to be different enough from the variant it belongs to, to be classified with its own label.
Immunity, vaccines, and variants
The differences between variants, sub-variants, and the original index virus have an impact on our immunity to infection and the ability of vaccines and past infections to help protect us.3 4 Because the earlier vaccines (e.g., Pfizer/Comirnaty, AstraZeneca, Moderna, Novavax) were developed based on earlier versions of SARS-CoV-2, they are not as effective in eliciting an immune response to newer variants including Omicron and its sub-variants. Likewise, past infection with an earlier variant helps train the immune system to recognise and respond to infection, however, if a new variant or sub-variant is different enough from the type that caused the previous infection, a strong immune response might not be triggered resulting in infection.
There is emerging evidence that booster doses of these vaccines provide a degree of protection against infection, severe illness, and death even for currently circulating sub-variants, so it remains recommended that those who can be vaccinated and are eligible, should consider getting a booster dose in accordance with their jurisdictional requirements.
As new vaccines that account for new variants and sub-variants are developed and rolled out, greater protection might be afforded against infection, developing severe illness, and death. In Australia, the Therapeutic Goods Administration (TGA) has provisionally approved Moderna’s bivalent COVID-19 vaccine, elasomeran/ imelasomeran (SPIKEVAX Bivalent Original/Omicron) for use as a booster dose in adults 18 years and over. While at the time of writing, the vaccine is not yet available, this is the first bivalent COVID-19 vaccine approved for use in Australia. Early analysis shows that this bivalent vaccine generates a higher immune response against the sub-variants BA.4 and BA.5 than the original SPIKEVAX vaccine.
‘Second generation’ COVID-19 vaccines are also under development that work differently in comparison to the earlier vaccines. These newer vaccines are anticipated to be better able to confer protection against future variants and some may be able to be delivered via a nasal spray rather than an intramuscular injection.5 Oral antivirals are another line of defence against COVID-19, however currently, these appear not to be widely utilised in Australia, so it is difficult to determine what part they have or will play in responding to future waves.6
Infectiousness and illness severity
As noted above, new variants and sub-variants are often more highly infectious in comparison to earlier variants due to mutations that make them better able to enter human cells and their propensity to colonise the upper airways resulting in a greater ability to be spread by expired air though coughing, sneezing, breathing, and talking.7 It is therefore important that infection prevention and control measures such as personal protective equipment (PPE), hand hygiene, and mask wearing and public health actions including quarantine/isolation requirements continue to be applied to protect particularly those who are most vulnerable to developing severe illness.
While new variants and sub-variants appear to be more highly transmissible, they also appear to cause less severe illness in most people.8 This is a typical evolution pathway for most infectious diseases, as it benefits the virus to infect as many people as possible without killing them. People who are vulnerable to developing severe illness, such as older adults and people with underlying conditions or disabilities are still at greater risk than most community members of developing severe COVID-19 illness and death, however. This means that while the overall impact of new waves of COVID-19 might be less and less over time, there are still people in the community who will become sick and potentially die as a result of infection.9
What’s next?
The trajectory of COVID-19 in Australia appears to indicate that waves appear approximately every three to four months and last for around one to two months from start to finish. This suggests that the next wave of infections is due to peak in mid-November to December 2022, which is around the same time that the Omicron wave began in 2021. At present, it is unclear what variant or subvariant will be the most common during this new wave, but it may be likely to be an Omicron sub-variant. Ensuring that people are up to date with their vaccination/booster schedule and that ongoing adherence to basic infection prevention and control and public health messages are the best ways to protect the health and wellbeing of the community and vulnerable members.
With the time that people must isolate/quarantine being reduced from seven days to five, it is likely that there will be a potential jump in the number of infectious people in the community, since evidence suggests that some people can continue to be infectious beyond five and even seven days following infection. At this stage, however, it is difficult to predict the full impacts of reduced isolation periods, as there are many complex and interrelating factors that influence the level and transmission of COVID-19 in Australia and abroad.
*ALERT* Evidence regarding COVID-19 is continually evolving. This resource will be updated regularly to reflect new emerging evidence but may not always include the very latest evidence in real-time.
References
-
Rubin R. COVID-19 Vaccines vs Variants—Determining How Much Immunity Is Enough. JAMA 2021;325(13):1241-43. doi: 10.1001/jama.2021.3370
-
Parums V. Editorial: Revised World Health Organization (WHO) Terminology for Variants of Concern and Variants of Interest of SARS-CoV-2. Med Sci Monit 2021;27:e933622. doi: 10.12659/msm.933622 [published Online First: 2021/06/22]
-
Altmann DM, Boyton RJ, Beale R. Immunity to SARS-CoV-2 variants of concern. Science 2021;371(6534):1103-04. doi: doi:10.1126/science.abg7404
-
Fiolet T, Kherabi Y, MacDonald C-J, et al. Comparing COVID-19 vaccines for their characteristics, efficacy and effectiveness against SARS-CoV-2 and variants of concern: a narrative review. Clinical Microbiology and Infection 2022;28(2):202-21. doi: https://doi.org/10.1016/j.cmi.2021.10.005
-
Acosta-Coley I, Cervantes-Ceballos L, Tejeda-Benítez L, et al. Vaccines platforms and COVID-19: what you need to know. Tropical Diseases, Travel Medicine and Vaccines 2022;8(1):20. doi: 10.1186/s40794-022-00176-4
-
Vitiello A, Ferrara F, Auti AM, et al. Advances in the Omicron variant development. Journal of Internal Medicine 2022;292(1):81-90. doi: https://doi.org/10.1111/joim.13478
-
Sheward DJ, Kim C, Fischbach J, et al. Evasion of neutralising antibodies by omicron sublineage BA.2.75. The Lancet Infectious Diseases doi: 10.1016/S1473-3099(22)00524-2
-
Madhi SA, Kwatra G, Myers JE, et al. Population Immunity and Covid-19 Severity with Omicron Variant in South Africa. New England Journal of Medicine 2022;386(14):1314-26. doi: 10.1056/NEJMoa2119658
-
Moore PL, Baden LR. Omicron — Decoupling Infection from Severe Disease. New England Journal of Medicine 2022;386(14):1361-62. doi: 10.1056/NEJMe2201812
Authors:
Micah DJ Peters PhD and Casey Marnie are at the National Policy Research Unit (Federal Office), Australian Nursing and Midwifery Federation (ANMF) and University of South Australia, Clinical and Health Sciences, Rosemary Bryant AO Research Centre