A new project is aiming to build a “digital health workforce” of nurses, doctors and allied health to better target the needs of people living with chronic diseases in low socioeconomic neighbourhoods by making virtual care and telemonitoring more efficient.
Led by Flinders University, the $1.1 million ‘safe@home’ hopes that providing affordable and effective primary care services will reduce ED and hospital admissions, GP clinic waiting times and ambulance ramping.
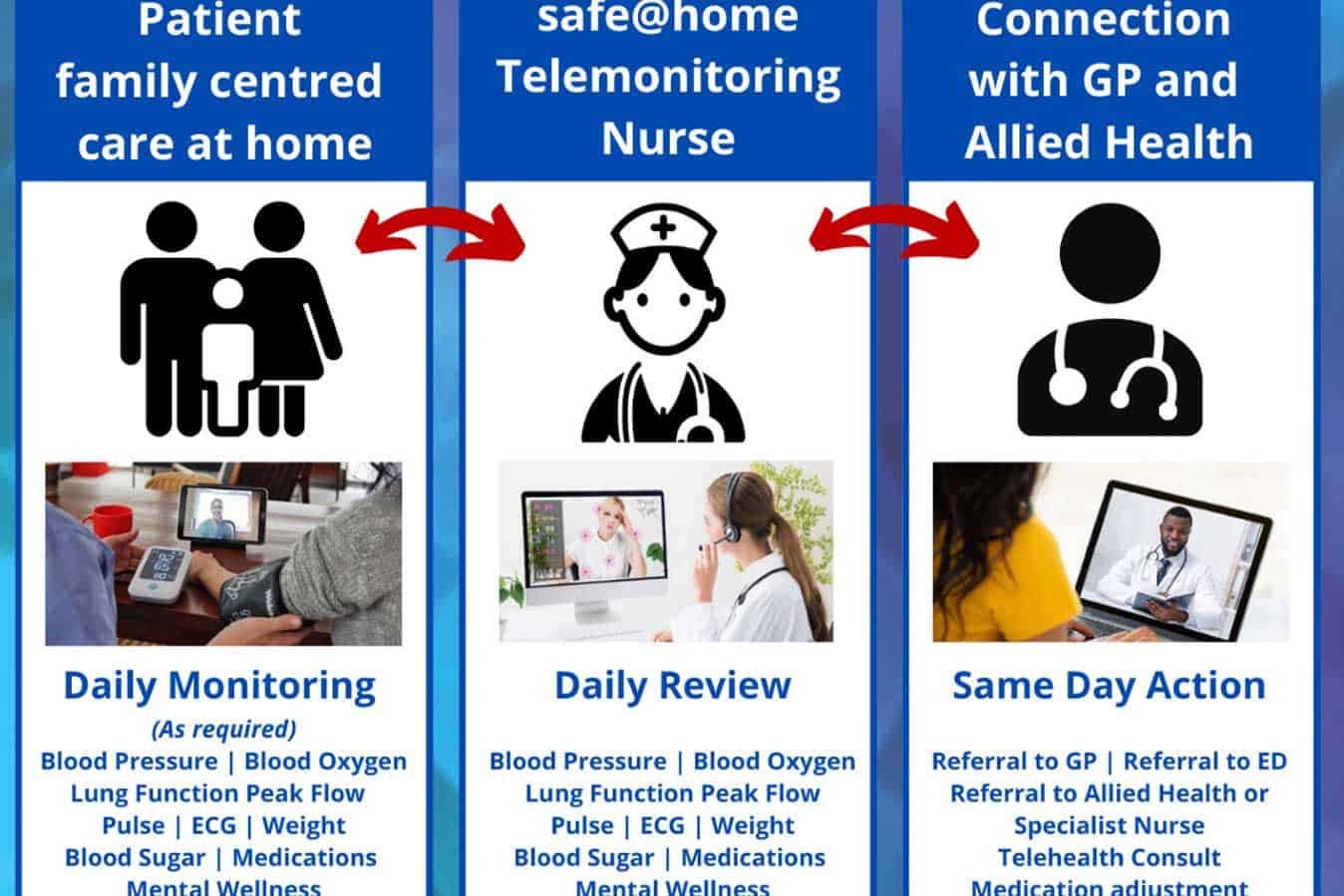
Home telemonitoring and virtual care will involve consumers in their model of care and give them incentive to increase their self-care and self-monitoring to manage their conditions, project leads say.
It also will be used to develop a business model using routine Medicare item numbers for primary care and a framework for scaling into routine care, including refinement of the interfaces with the electronic medical records and patients’ clinics. Chief investigator – Caring Futures Institute Flinders University Professor Robyn Clark, from the College of Nursing and Health Science – will work with key public health groups across the Adelaide metropolitan area on the initiative with funding from a National Health and Medical Research Council (NHMRC) Partnership Project announced today.
SA Health and other agency involvement includes the Northern Adelaide Local Health Network, the Adelaide Primary Health Network, Australian Telehealth Society, Digital Health SA and Integrated Cardiovascular Clinical Network SA.
“With the unrelenting pressure on our healthcare system, and ageing population, we will be focusing on creating a robust primary care framework for people living with high needs, such as heart failure, diabetes, hypertension and chronic obstructive pulmonary disease (COPD),” says Professor Clark, a Professor of Acute Care in Cardiovascular Research with the Caring Futures Institute at Flinders University. “Along with providing quality care in the home setting, we aim to improve the everyday quality of life for these patients by giving them more regular health checks and access to professional help.”
“Even more than this monitoring, it is the clinical decisions and actions taken based on information obtained by monitoring that will alter patient wellbeing and outcomes.”
Dr John Maddison, the Executive Director of Medical Services at the Northern Adelaide Local Health Network, said the venture was a positive development.
“Embracing technology and linking General Practice with Hospital Care is the best way to keep our patients safe at home, which is better for patients and also helps take the pressure off our emergency departments,” he said.








