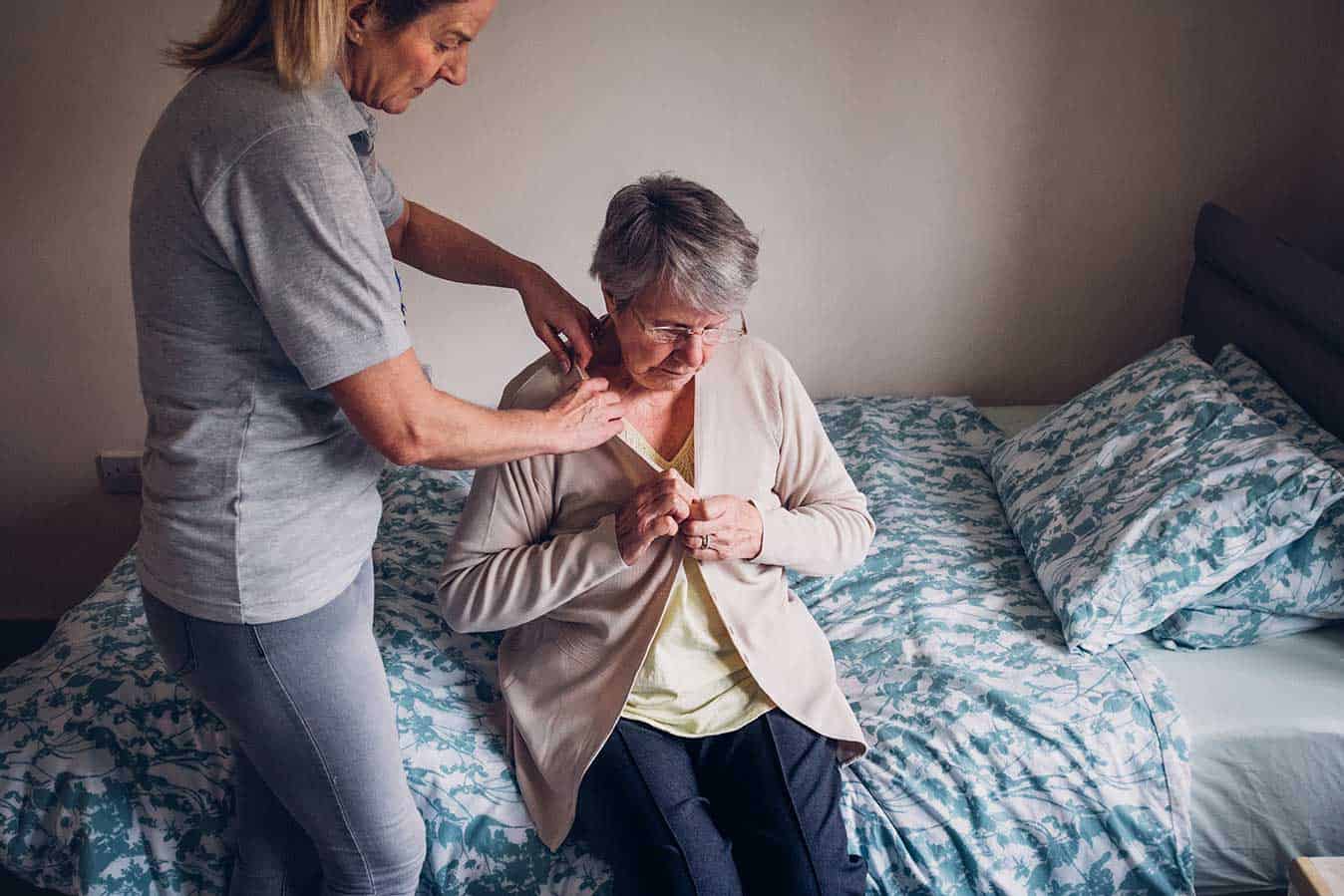
Aged care workers are so rushed and under pressure to provide basic physical care for the elderly that they have no time left to meet important social and emotional needs, a joint UNSW Sydney, Macquarie University and RMIT study has found.
The research showed aged care workers have insufficient time to talk to and get to know their residents or support their decision-making and independence.
Lead author Professor Gabrielle Meagher, from Macquarie University’s Department of Sociology said evidence had long shown older people value the relationships they forge in aged care and consider quality services to be those where staff have the time and flexibility to get to know them and attend to their needs.
But it has become structurally difficult to provide this level of care, she added.
“The Australian aged care system has to meet increasing levels of demand, and to respond to the increasing complexity of need among older people related to daily living, behavioural issues or complex healthcare. Our research shows this has not been matched with appropriate funding, staffing levels or a mix of staff skills.”
Published last October, the Meeting the social and emotional support needs of older people using aged care services report, prepared for the Health Services Union and United Voice, found:
- The number of aged care places has outstripped workforce growth, with no increase in the ratio of full-time equivalent care workers to residential care places since 2003.
- Personal Care Workers perform an increased amount of direct care work in residential settings, up from 57% in 2003 to 72% in 2016, while the share of nurses and allied health professionals has declined.
- 90% of care workers across residential and home care services reported having no time to respond to unexpected needs, or to spend time with an older person considered in low spirits.
- 78% said they had insufficient time to support older people to do things for themselves, such as use a walker instead of a wheelchair.
- Just 37% felt their managers understood the importance of workers’ relationships with older people, with many reporting they believed they were looked upon as “slacking off” if they attended to a client’s social and emotional needs.
“Care workers routinely observe that older people’s emotional needs are left unmet in the system designed to support them,” Wendy Taylor, from RMIT’s School of Management, said.
“In the aged care system today, overlooking older people’s basic social and emotional needs has become part of accepted business practices.”
The research also found limited organisational support for quality care, with less than 22% of aged care workers receiving one-on-one support from a supervisor and less than half being given the opportunity to take part in meetings to discuss how care is provided.
“Insufficient time and support for relationship building and care makes it difficult to realise principles of dignity, respect and person-centredness in aged care. This partially explains the very high rates of social isolation and mental distress experienced by older people,” Professor Meagher argued.
“Employment conditions and pay rates in aged care also fail to recognise the specific skills and demands of the work, leaving care workers and older people vulnerable,” RMIT’s Professor Sara Charlesworth added.
The report made a range of recommendations, including the need to consider the psychosocial needs of older people when designing aged care services, increased aged care funding in order to provide all older people with person-centred care, and improved staffing arrangements to allow workers enough time to care and offer continuity of care relationships.
It also called for workers to have relevant practice and relational skills to deliver high-quality care and be better supported by managers to allow them to develop meaningful relationships with residents.








One Response
This is why as an acute care AIN working in a hospital I get so much more job satisfaction than working in a nursing home. Some days are flat out but other days I have the time to spend just talking to patients, particularly the elderly or those going through a really hard time. I’m sure it won’t last though… the powers that be will decide if we have time for that then we’re wasting time. But I’m enjoying it while it lasts.